What is an addiction?
What is an addiction?
To start, let’s distinguish between two types of addiction². There are substance use addictions and behavioral addictions.
Substance use addictions are those we might typically think of when we hear the word addiction; it includes substances like alcohol, caffeine³, cannabis, hallucinogens, opioids, sedatives, stimulants, and tobacco. It’s not that these substances are inherently bad⁴ – but when used compulsively, they become problematic because they can rob one of their self-worth and freedom to choose.
On the other hand, behavioral addictions include activities that people engage in that can become compulsive and therefore problematic. Gambling or pornography use for example, can be considered a behavioral addictions⁵. However, there’s some debate on what else constitutes a behavioral addiction. For example, problematic internet use, compulsive shopping or excessive sexual behavior are not officially recognized diagnoses⁶. However in my opinion, they can become no less addictive than substances.
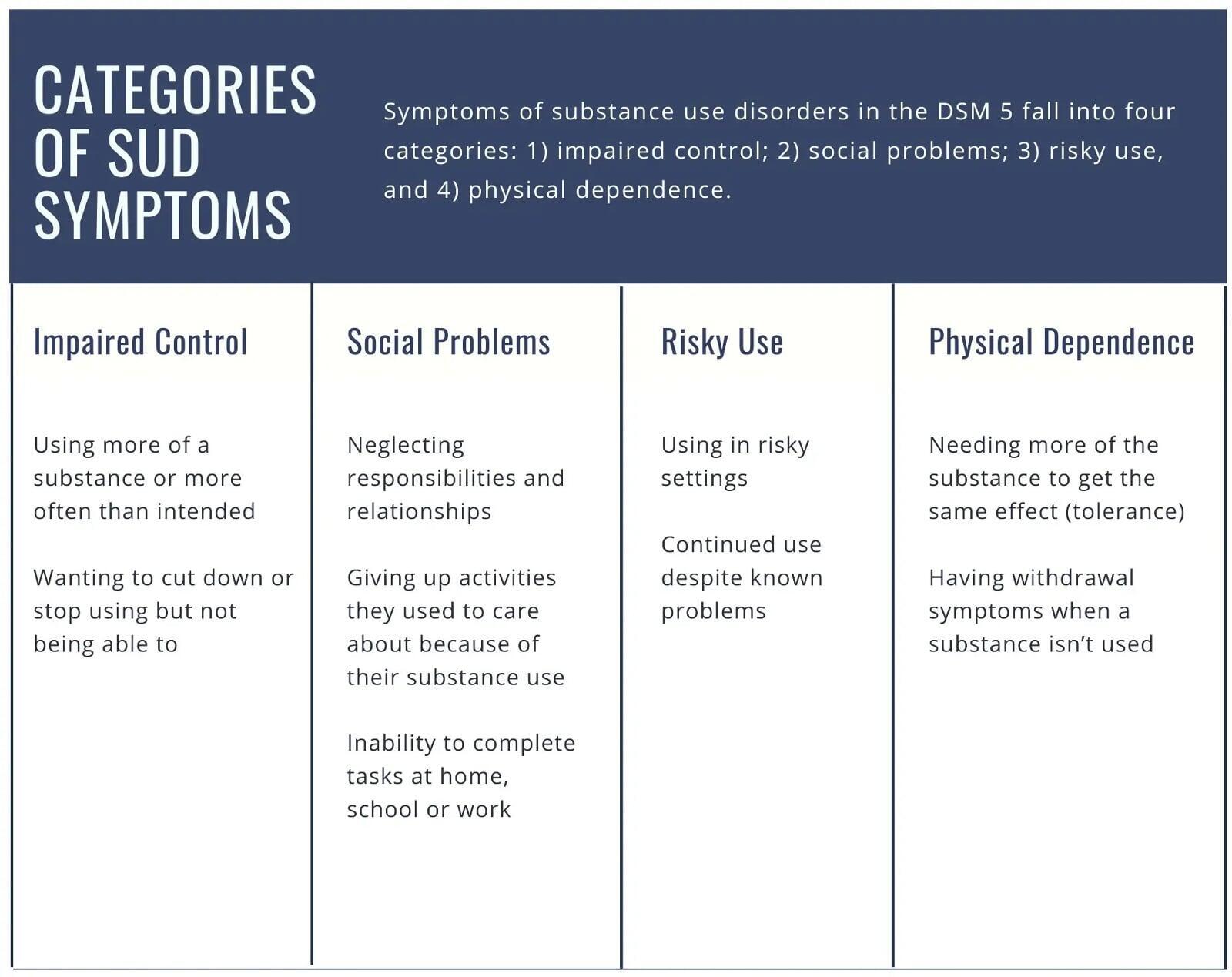
To diagnose someone with a substance use disorder, certain criteria need to be met⁷ per the American Psychological Association (APA). Generally, these criteria fall into four categories (as shown in the infographic below): impaired control, social problems, risky use, and physical dependence⁸.
Addiction occurs on a spectrum.
Any two or three symptoms are indicative of a mild substance use disorder.
Any four or five symptoms are indicative of a moderate substance use disorder.
And any six or more symptoms are indicative of a severe substance use disorder, also known as an addiction⁹.
It might be easy to review this list and get caught up on labeling and self-diagnosis¹⁰. Let’s try and not go down that road because there’s more nuance to this¹¹.
Why do we get addicted?
Why do we get addicted?
Before we get into how to recover from an addiction, it’s important to understand why addiction occurs in the first place. There are several schools of thought on this¹². But in my opinion, addiction most often begins when an individual is in pain.
That pain drives the individual – unknowingly or not – to self-medicate with substances or behaviors that soothe the emotional or physical distress.
When the substance or behavior is indulged, the brain is rewarded with a flood of neurotransmitters (dopamine, glutamate etc.)¹³ which allow the individual to experience pleasure and, in some sense, self-regulate in the short-term.
Over time however, the brain learns to seek out these substances and behaviors under conditions of distress. This cycle of pain management begins to impact the individual’s decision-making processes at a neurobiological level, as their agency becomes increasingly hampered. What begins as a coping mechanism becomes maladaptive over time. And with increased stress comes increase craving.
The person caught in this trap is never quite able to soothe their real pain through the substance or behavior. As a result, often more is needed. Eventually the distraction becomes a preoccupation. And so the addiction begins to tightening its grip.
It is important to note that the addiction itself is not genetically predetermined¹⁴. Rather genetic and environmental factors can influence how vulnerable or susceptible an individual is.
In short, addiction has its roots in both neurobiological factors and environmental influences. Understanding this is key to breaking the addictive cycle.
How to recover from an addiction
How to recover from an addiction
In my clinical experience, successfully treating addiction requires getting to the root cause of the distress that may be driving the addictive cycle. If we can properly treat that pain, we effectively cut off the fuel for the addiction.
For many that find themselves addicted, early developmental trauma often seems to be the culprit. This isn’t a blanket statement because addiction is complex¹⁵. However, there are plenty of data that demonstrate a connection between childhood trauma and addiction¹⁶.
The landmark ACE (Adverse Childhood Experiences) study¹⁷ looked at the incidence of painful experiences in the lives of over 17,000 people. These painful experiences included family violence, parental divorce, drug or alcohol abuse in the family, death of a parent, and physical, emotional or sexual abuse.
The researchers found a compelling correlation between these early adverse experiences and substance abuse later in the subjects’ lives. “For each adverse childhood experience, or ACE, the risk for the early initiation of substance abuse increased between two- and fourfold. Subjects with five or more ACEs had seven to ten times greater risk for substance abuse than those with none¹⁸”.
While I’m not suggesting that everyone struggling with an addiction has early childhood trauma, my experience (and the literature) indicates that it is this early childhood trauma that makes one susceptible to all kinds of addictions later on in life.
This is why I don’t necessarily see an addiction as the problem itself, but rather a symptom of unseen wounds.
While there’s no magic pill that can cure addiction, there are some promising medications and treatments that can help facilitate recovery¹⁹. Even so, if we can process through that trauma together to treat those emotional wounds, we may find that the addiction — whether it be substance use or behavioral — begins to fade on its own.
Final Thoughts
Final Thoughts
I have never been a fan of the term addict. In many ways, people that struggle with addictions are not so different than anyone else. We simply don’t know what someone else’s life has been like. We don’t know the burdens that others carry — so the best policy is to be kind to everyone. When you’re struggling with addiction, the last thing you need is someone’s judgment.
A few other observations from my clinical experience:
Addiction thrives in secrecy. If you’re struggling with an addiction, find someone you trust to confide in. You’re not alone.
Sometimes time doesn’t heal wounds, but rather allows them to fester. The sooner individuals seek treatment, the sooner they find relief.
Sometimes sheer will and grit aren’t enough. Until we get to the root of the addiction, it will feel like an uphill battle.
Nobody wants to be addicted. Addiction is not the result of a moral failing. One’s will can quite literally be overridden with an addiction²⁰.
An addiction is not an indicator of moral character.
It’s not your fault. Understanding that addiction often has roots in early childhood trauma can be freeing in some sense. But at the same time, this doesn't exempt individuals from being accountable for their own lives.
Everyone could use help from time to time. If you feel stuck trying to kick a bad habit, know that there’s hope.
- Highlights from the 2022 National Survey on Drug Use and Health. (2023). In Substance Abuse and Mental Health Services Administration. Substance Abuse and Mental Health Services Administration. Retrieved January 25, 2024, from https://www.samhsa.gov/data/sites/default/files/reports/rpt42731/2022-nsduh-main-highlights.pdf
- There are also substance induced disorders, but that’s beyond the scope of what we’ll talk about.
- Meredith, S. E., Juliano, L. M., Hughes, J. R., & Griffiths, R. R. (2013). Caffeine Use Disorder: A Comprehensive Review and Research Agenda. Journal of caffeine research, 3(3), 114–130. https://doi.org/10.1089/jcr.2013.0016
- Many of these substances have medical purposes.
- American Psychological Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
- Grant, J. E., & Chamberlain, S. R. (2016). Expanding the definition of addiction: DSM-5 vs. ICD-11. CNS spectrums, 21(4), 300–303. https://doi.org/10.1017/S1092852916000183
See footnote #5
- McNeely, J. (n.d.). Table 3, DSM-5 Diagnostic Criteria for Diagnosing and Classifying Substance Use Disorders [abc] - Substance Use Screening and Risk Assessment in Adults - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK565474/table/nycgsubuse.tab9/
- Addiction Policy Forum (2022, October 19). DSM-5 Criteria for Addiction Simplified. APF. https://www.addictionpolicy.org/post/dsm-5-facts-and-figures
- More frequently I’ve been running into clients coming in with self-proclaimed diagnoses. I find this can hamper the therapeutic process for a number of reasons. Honestly, this topic could be its own post. Caron, C. (2022b, October 29). Young people on TikTok are Self-Diagnosing. The New York Times. https://www.nytimes.com/2022/10/29/well/mind/tiktok-mental-illness-diagnosis.html
- The DSM-5 considers these criteria guidelines. It’s up to the clinician to determine the best course of treatment. To diagnose a substance use disorder, a healthcare provider may also take a medical history and have the client complete a physical exam or other tests (blood, urine etc.).
- There are many ways to look at addiction. There are certainly genetic, epigenetic, biological, cognitive, behavioral, social, environmental and psychodynamic factors that come into play.
- Semaan A, Khan MK. Neurobiology of Addiction. [Updated 2023 Nov 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK597351/
- Substance Abuse and Mental Health Services Administration (US); Office of the Surgeon General (US). Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health [Internet]. Washington (DC): US Department of Health and Human Services; 2016 Nov. CHAPTER 2, THE NEUROBIOLOGY OF SUBSTANCE USE, MISUSE, AND ADDICTION. Available from: https://www.ncbi.nlm.nih.gov/books/NBK424849/
- See footnote#10
- Khoury, B., Tang, Y., Bradley, B., Cubells, J., & Ressler, K. J. (2010). Substance use, childhood traumatic experience, and Posttraumatic Stress Disorder in an urban civilian population. Depression and Anxiety, 27(12), 1077–1086. https://doi.org/10.1002/da.20751
- About the CDC-Kaiser ACE Study |Violence Prevention|Injury Center|CDC. (n.d.). https://www.cdc.gov/violenceprevention/aces/about.html
- Máté, G. (2012). Addiction: Childhood Trauma, Stress and the Biology of Addiction. Journal of Restorative Medicine, 1(1), 56–63. https://doi.org/10.14200/jrm.2012.1.1005
- Fairbanks, J., Umbreit, A., Kolla, B. P., Karpyak, V. M., Schneekloth, T. D., Loukianova, L. L., & Sinha, S. (2020). Evidence-Based Pharmacotherapies for alcohol use Disorder. Mayo Clinic Proceedings, 95(9), 1964–1977. https://doi.org/10.1016/j.mayocp.2020.01.030
- This book illustrates an example of this. Pond, M., & Palmer, M. (2016). Wasted: An alcoholic therapist’s fight for recovery in a flawed treatment system. Greystone Books.